
Mr J Compton
Chief Executive
Health and Social Care Board
12-22 Linenhall Street
Belfast
BT2 8BS
28 February 2012
Dear Mr Compton
External Clinical Adviser
With reference to your letter dated 23 February 2012, please find responses to questions as follows:
1. What is your assessment of the clinical communication and collaboration across the primary/secondary care interface?
Trust and primary care colleagues have not yet achieved robust and resilient communication and collaboration. There is clear goodwill and resolve to achieve this in primary and secondary care.
At grassroots level, many hospital clinicians describe good communication with GPs but this is acknowledged to be patchy – difficulties with access during the busy working day and relatively limited IT support for real time communication are cited as the main reasons. The last two and a half years, during the accelerated reconfiguration of two of our smaller acute sites, have been a particularly difficult and disruptive time with multiple personnel changes at consultant level across the locality, changing access to services and irregular clinic schedules: this scenario is now stabilising. Consultants are very eager to improve communication as the benefits for both patient care and clinical effectiveness are clear.
Following the hospital reconfiguration, the HSCB commissioned ‘Tribal’, a healthcare consultancy to conduct a study of unscheduled care capacity and utilisation. The review report, broadly accepted by the Trust, with reservations on timelines for achieving change, recommended a number of significant changes in care patterns. These included the development of ambulatory care pathways within secondary care, with protocol-driven direct access for GPs. There was considerable engagement of primary care colleagues, and expectations were raised of material change by November 2011. Secondary care colleagues were unhappy with the quality of the final draft pathways presented, and the initiative did not proceed. This has caused considerable disappointment and frustration in both primary and secondary care. The Trust is taking forward work on pathways and associated developments, and has sought support from NI Safety Forum and other quarters to support further joint improvement work. Primary care colleagues are aware of these plans and have continued to engage with them.
There is recognition of shared responsibility to improve the primary-secondary interface and this has gained considerable momentum this year in the wake of a range of small shared initiatives to re-design services across traditional boundaries.
The standing ‘GP Forum’ was redesigned in the last year, with supporting ‘locality’ forums created and the groups reconstituted to foster improved communication across primary, Trust managed community care and secondary care teams. Initial feedback is that these new fora are working well, but have been in place for a matter of months only at this time. Some concerns have been identified at the fora, and improvement plans have been developed in response. (See minutes of meetings, already forwarded).
There has been a positive approach to clinical engagement in planning for ‘Transforming Your Care’ with the setting up of Professional Advisory Groups which are co-chaired by GPs (Appendix 1).
2. How can a shared culture of continuous improvement of patient safety, quality of care and patient experience be promoted, both within the Trust and across the primary/secondary care interface?
The Trust has a positive history of engaging in safety and quality focussed work, including participation in Safer Patient Initiative 2 and the Trust continues to be an active participant in the Safer Patient Network. This work is taken on through the Patient Safety and Quality Improvement Plan (PSQIP) (Appendix 2) and progress on this is reported to the Governance Management Board (GMB) and to Trust Board through regular progress reports (Appendix 3).
The Trust had an outbreak of C Difficile in 2008 that led to a public inquiry that reported in late 2010. The learning from that process and the report that followed has shaped the Trust’s response to quality and safety, and the focus on each patient’s experience in particular. A dedicated Executive Director of Nursing and Patient Experience has been appointed, a broad range of action plans are in place to address the concerns identified by the experience of the outbreak, and highlighted by the inquiry (Appendix 4).
A range of quality improvement work in the nursing domain is now in place, and continues to develop.
The medical leadership and engagement process has been reviewed, and a revised structure and supporting processes are in place. There is a significant agenda on clinical leadership development, and on the further development of multi-disciplinary governance, and there is a clear appetite for engagement. (Information on these areas has already been forwarded).
The HSCB Safety Forum (SF) is promoting spread of IHI methodology in the region by sponsoring places on the IHI Open school program. A number of our staff have availed of this opportunity and we continue to actively promote participation - the Trust has confirmed that it will fund additional places for any interested clinical staff. Nurse and consultant teams are to undergo Global Trigger Tool Training during the course of this year; this event is also sponsored by the SF.
The monthly Acute Directorate Consultants (Safety and Quality) Forum has been discussing safety and risk in secondary care – at their last meeting they were joined by the HSCB’s Assistant Director for Integrated Services. Next month is to be a joint meeting with GP colleagues looking at incident/event reporting to change the way this is perceived and to build a safety culture.
The HSCB Safety Forum has offered to host a primary-secondary collaborative for Northern Area clinicians on pathways for unscheduled/ urgent access a part of its regional Emergency Medicine Safety Collaborative program. This is being explored with the Dalriada Urgent Care (the local out of hours GP service) and we anticipate that work will commence in early April.
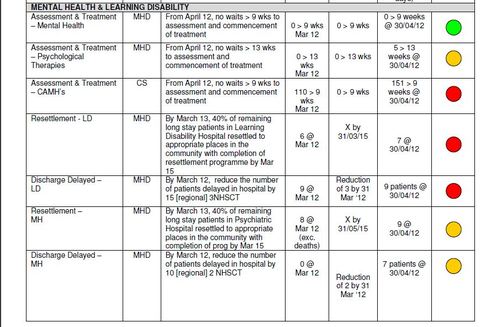
Improvement work on unscheduled care and in other service areas including Mental Health, Learning Disability and Children’s Services is focussed on promoting safe and effective patient or client journey.
3. How can clinical safety and quality improvement be supported and measured, both from within the Trust and across the primary/secondary care interface. How can any concerns in this regard be addressed?
It is recognised that safety and quality improvement across the system must be owned and delivered by frontline staff. This requires a supportive infrastructure including organisation and goal-setting, shared learning and openly-shared transparent data to monitor system change. The current engagement of clinical staff via Professional Advisory Groups (Appendix 1), which have been set up to assist the LCG/Trust with its response to Transforming Your Care, should provide a platform for this work. The option for shared small change cycles is built into the consultation.
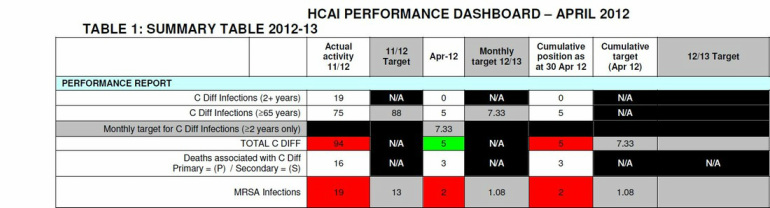
The Trust is developing a Safety and Quality Ward Dashboard to collate and share improvement metrics in a way that is clinician-friendly by being light on process. An offline version should be in place by April and we aim to make it available on line within 2012 if clinicians can be confident its data quality.
With reference how concerns are expressed across the interface, the responses in (1) and (2) - i.e. improved day to day communication and the growth of a safety culture should improve on the current situation.
In addition to this approach, primary care reports adverse incidents to the Trust. Approximately 20 such incidents are reported per year and the main issues are Estates problems in Trust owned Health Centres, communication difficulties related to discharge and medication issues. The Trust is working with colleagues in the HSC Board to revise this process so that concerns raised about the primary/secondary care interface can be jointly reviewed and addressed in a way that promotes learning and avoids any form of “blame culture”.
The Trust continues to actively develop Clinical Audit and has recently established a new Audit and Effectiveness committee with a view to ensuring stronger clinical engagement with this process (Appendix 5).
Incidents and Complaints Management support this function. Datix risk management system is the database used to capture this information. Incidents and complaints reports are monitored and reviewed regularly by the Governance Management Board to identify trends/patterns and learning (See Appendix 6 - Complaints Annual Report, and Appendix 7 - two quarterly reports).
4. How does the Trust secure feedback from Patients?
- Through the complaints management process (Appendix 8 Complaints Policy):
- The Complaints and Service User Feedback Policy invites comments, suggestions, compliments and complaints from those who use our service. The feedback can be given by email, phone, written, Trust website and through the Trust Feedback leaflet "Your views matter" (Appendix 9). The Trust leaflet is available on the Trust website and across all locations within the Trust including community settings for clients/patients/relatives/visitors to access.
- Patient Experience/Feedback is being captured through the Patient Safety Leadership Walkrounds. These walk-rounds are undertaken every month by Trust Directors and Assistant Directors. This information is collated/ actioned and is presented to GMB (Appendix 10 LW Proforma).
- Regional Patient Experience reports - Audits are undertaken every quarter in specific areas across the Trust. This programme is set regionally and reports to the PHA. The audits have 3 elements - Patient Experience, Patient Stories and Observations. The audit results are presented to GMB every quarter. (Copies of these reports have already been forwarded).
- Patient Experience – a range of mechanisms are in place to gain feedback from users and carers on service experience and on development proposals. These include a long-standing Older People’s panel, which contribute to strategic development and to service specific change debate, including the development of the Older Persons’ pathway. There is well-developed user involvement in Cancer services, Endoscopy services and a range of other services.
Dr P Flanagan
Medical Director
Encs.
 RSS Feed
RSS Feed
